We collected patients with thrombocytopenia after chimeric antigen receptor (CAR)T cell therapy for non-Hodgkin lymphoma in our center, and retrospectively analyzed the clinical characteristics of methylprednisolone for the treatment of thrombocytopenia after (CAR)T cell therapy .The primary objective was to evaluate the efficacy and safety of long-term step-reduced methylprednisolone in patients with severe persistent thrombocytopenia(Thrombocytopenia ≥ grade 3, duration≥2 weeks) after CAR-T cell therapy.
This study retrospectively analyzed patients with non-Hodgkin lymphoma who received chimeric antigen receptor (CAR) T cell therapy in Tongji Hospital Affiliated to Tongji University from November 2018 to July 2023. 34 patients developed thrombocytopenia during treatment and follow-up,5 patients lost to follow-up;1 patient died of COVID-19 pneumonia;10 patients with thrombocytopenia after CAR-T cell therapy had poor response to TPO-RA, blood transfusion, and methylprednisolone, all of them progressed rapidly due to poor efficacy of CAR T cell therapy. The other 18 (CAR) T cell therapy patients with thrombocytopenia were all CR(Complete remission) assessed after 3 months (Table 1).
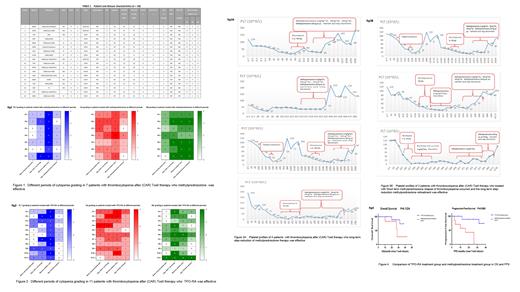
Further analysis of the 18 patients with thrombocytopenia after (CAR) T cell therapy. The median follow-up period was 11.29 months (range,2.7 to 25.4 months), the lowest platelet count occurred 27.3 days (range, 4-106 days) after (CAR) T cell therapy. The incidence of grade 3-4 thrombocytopenia was 100%, and the incidence of grade 4 thrombocytopenia was 66.7%. The incidence of thrombocytopenia before (CAR) T cell therapy was 55.6%, all of them were grade 1-2 thrombocytopenia. Among them,11 patients with grade 3-4 thrombocytopenia with a duration<2 weeks were effective of TPO-RA and platelet transfusion(Figure 1).7 patients with grade 3-4 thrombocytopenia with a duration≥2 weeks did not respond to treatment with TPO-RA or platelet transfusion, but long-term step-reduction methylprednisolone was effective (Figure 2).
7patients with thrombocytopenia who did not respond to TPO-RA or platelet transfusion,and were finally effective in methylprednisolone were further analyzed. The initial prednisone dose of methylprednisone was 1mg/kg/ day for 5-7 days, The dose was reduced step by step until platelets recovered to grade 1(Figure 3A).the median response time of the treatment was 16.6 days (range,6-30 days). Among them, 3 patients treated with methylprednisolone at a dose of 1mg/kg/ day for 5 day and then stop,after the discontinuation of methylprednisolone, relapse of thrombocytopenia occurred and the symptoms were relieved again after long-term step-reduction methylprednisolone treatment (Figure 3B). Apart from drug-controlled hyperglycemia and hypertension, we observed no other side effects of prednisone.
Further, we found the median OS of the 7 patients who were treated with methylprednisolone was 28 months, and the median OS of the 11 patients who responded to TPO-RA was undefined (95% confidence interval 0.5296 to 25.06), with no significant difference in OS between the two groups (P=0.1224)(Figure 4) .The median PFS of the patients who were treated with methylprednisolone was 16 months, and the median PFS of the 11 patients who responded to TPO-RA was undefined (95% confidence interval 1.253 to 34.54), with a significant differences in PFS between the two groups (P=0.0063) (Figure 4).
Studies have shown that long-term step-reduction methylprednisolone is effective in severe persistent thrombocytopenia (Thrombocytopenia ≥ grade 3, duration≥2 weeks) .There was no significant difference in OS between the the patients who did not respond to TPO-RA, platelet transfusion,and were finally treated with methylprednisolone and the patients who responded to TPO-RA, platelet transfusion, but PFS of the patients were treated with methylprednisolone was shorter, suggesting that severe and persistent thrombocytopenia may be related to disease progression.
Disclosures
No relevant conflicts of interest to declare.